What an Atopic Dermatitis Rash looks like? Explore Symptoms and Remedies
Understanding Atopic Dermatitis
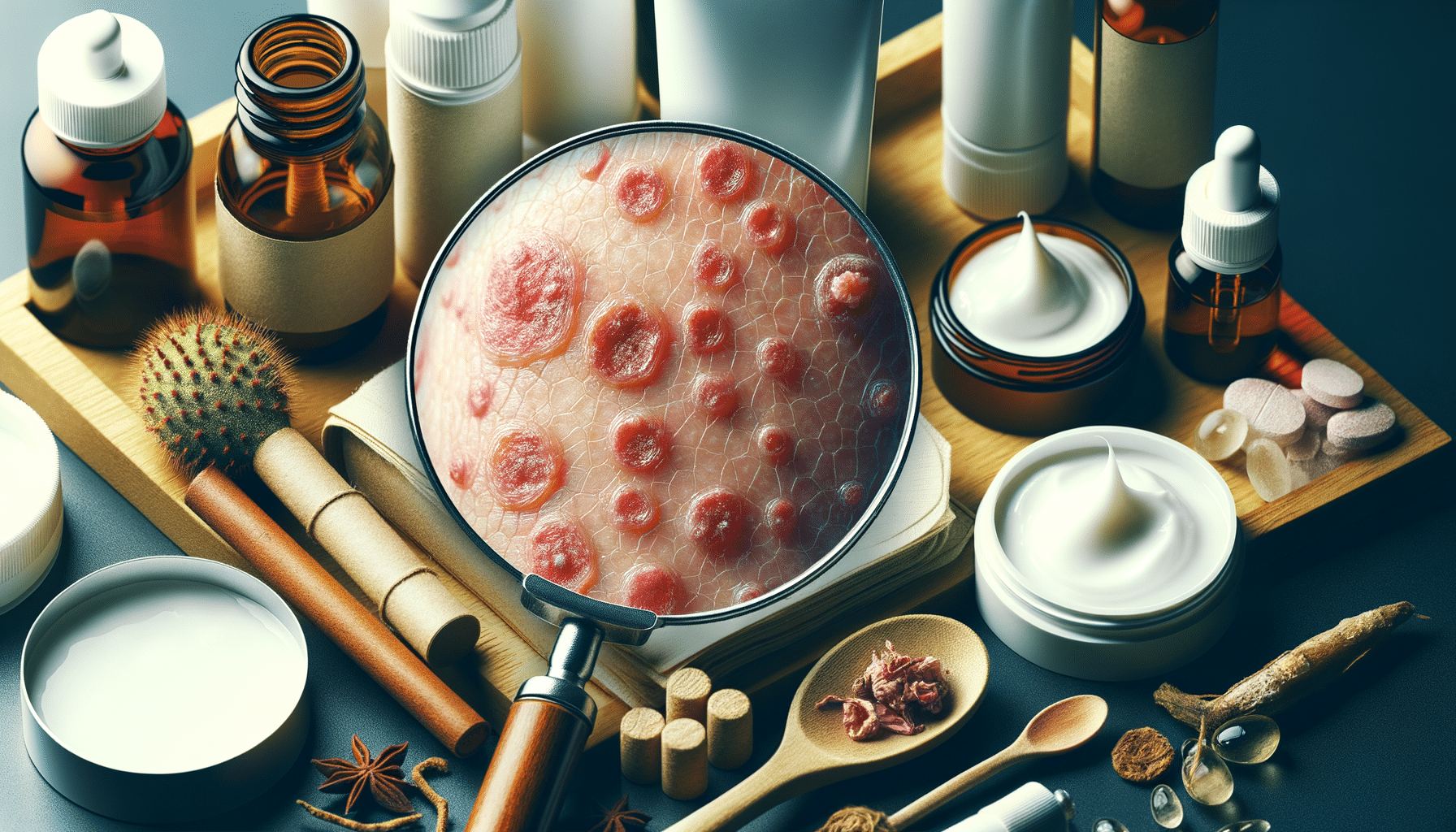
Atopic dermatitis, commonly referred to as eczema, is a chronic inflammatory skin condition that affects millions worldwide. Characterized by red, itchy rashes, this condition can significantly impact one’s quality of life. The term “atopic” refers to a genetic tendency to develop allergic diseases, and “dermatitis” means inflammation of the skin. Understanding the nature of atopic dermatitis is crucial for effective management and treatment.
Atopic dermatitis often begins in childhood, with symptoms appearing as early as infancy. However, it can also develop in adults, with varying severity. The condition is not contagious, but it can be hereditary, meaning if a family member has it, others might be more susceptible. The skin of those with atopic dermatitis is more sensitive to irritants and allergens, leading to the characteristic flare-ups.
Several factors can trigger or worsen atopic dermatitis. These include environmental factors like pollen, dust mites, and pet dander, as well as lifestyle factors such as stress and certain foods. The skin’s barrier function is compromised in individuals with atopic dermatitis, making it less effective at retaining moisture and more prone to irritation.
Symptoms and Diagnosis
The symptoms of atopic dermatitis can vary widely among individuals, but common signs include dry, scaly skin, intense itching, and red or brownish patches. These patches often appear on the face, inside the elbows, behind the knees, and on the hands and feet. During flare-ups, the affected areas may become swollen, cracked, or develop blisters.
Diagnosis of atopic dermatitis is primarily based on the physical examination of the skin and the patient’s medical history. Dermatologists look for the classic symptoms and may inquire about family history of allergies or asthma, as these are often linked. In some cases, patch testing or skin biopsy may be conducted to rule out other skin conditions.
It’s important to differentiate atopic dermatitis from other skin issues such as psoriasis or contact dermatitis, as the treatment approaches may differ. Early diagnosis and intervention can help manage symptoms effectively and prevent complications such as skin infections.
Triggers and Risk Factors
Understanding the triggers and risk factors of atopic dermatitis is essential for managing the condition. Common triggers include:
- Environmental allergens like pollen, dust, and mold
- Skin irritants such as soaps, detergents, and fragrances
- Weather changes, particularly dry or cold climates
- Stress and emotional factors
- Certain foods, especially in children, like eggs, milk, peanuts, and soy
Risk factors for developing atopic dermatitis include a family history of eczema, hay fever, or asthma. Individuals with a genetic predisposition to allergic reactions are more likely to experience this condition. Additionally, living in urban areas with higher pollution levels and less exposure to natural environments can increase the risk.
Recognizing and avoiding triggers is a key strategy in managing atopic dermatitis. Keeping a symptom diary can help identify specific triggers and aid in developing a personalized management plan.
Treatment Options
Treating atopic dermatitis involves a combination of lifestyle modifications, skincare routines, and medical interventions. The primary goal is to alleviate symptoms and prevent flare-ups. Here are some common treatment options:
- Moisturizers: Regular use of emollients helps maintain skin hydration and strengthen the skin barrier.
- Topical corticosteroids: These are anti-inflammatory creams or ointments prescribed to reduce redness and itching during flare-ups.
- Calcineurin inhibitors: These are non-steroidal medications used to suppress the immune response and control inflammation.
- Antihistamines: These can help relieve itching, especially at night.
- Phototherapy: Exposure to ultraviolet light under medical supervision can be beneficial for some individuals.
In severe cases, systemic medications like corticosteroids or immunosuppressants may be prescribed. It’s crucial to follow a dermatologist’s guidance and avoid overuse of topical steroids to prevent side effects.
Preventive Measures and Lifestyle Tips
Adopting preventive measures and lifestyle changes can significantly reduce the frequency and severity of atopic dermatitis flare-ups. Here are some effective strategies:
- Maintain a consistent skincare routine with gentle, fragrance-free products.
- Avoid hot showers and opt for lukewarm water to prevent skin drying.
- Wear soft, breathable fabrics like cotton and avoid wool or synthetic materials.
- Use a humidifier during dry seasons to maintain indoor moisture levels.
- Manage stress through relaxation techniques such as yoga or meditation.
Dietary changes may also play a role, particularly for those with food sensitivities. Consulting a nutritionist can help identify potential dietary triggers. Educating oneself about the condition and staying informed about new treatment options can empower individuals to take control of their skin health.