Understanding Autoimmune Skin Conditions: A Comprehensive Overview
Introduction to Autoimmune Skin Conditions
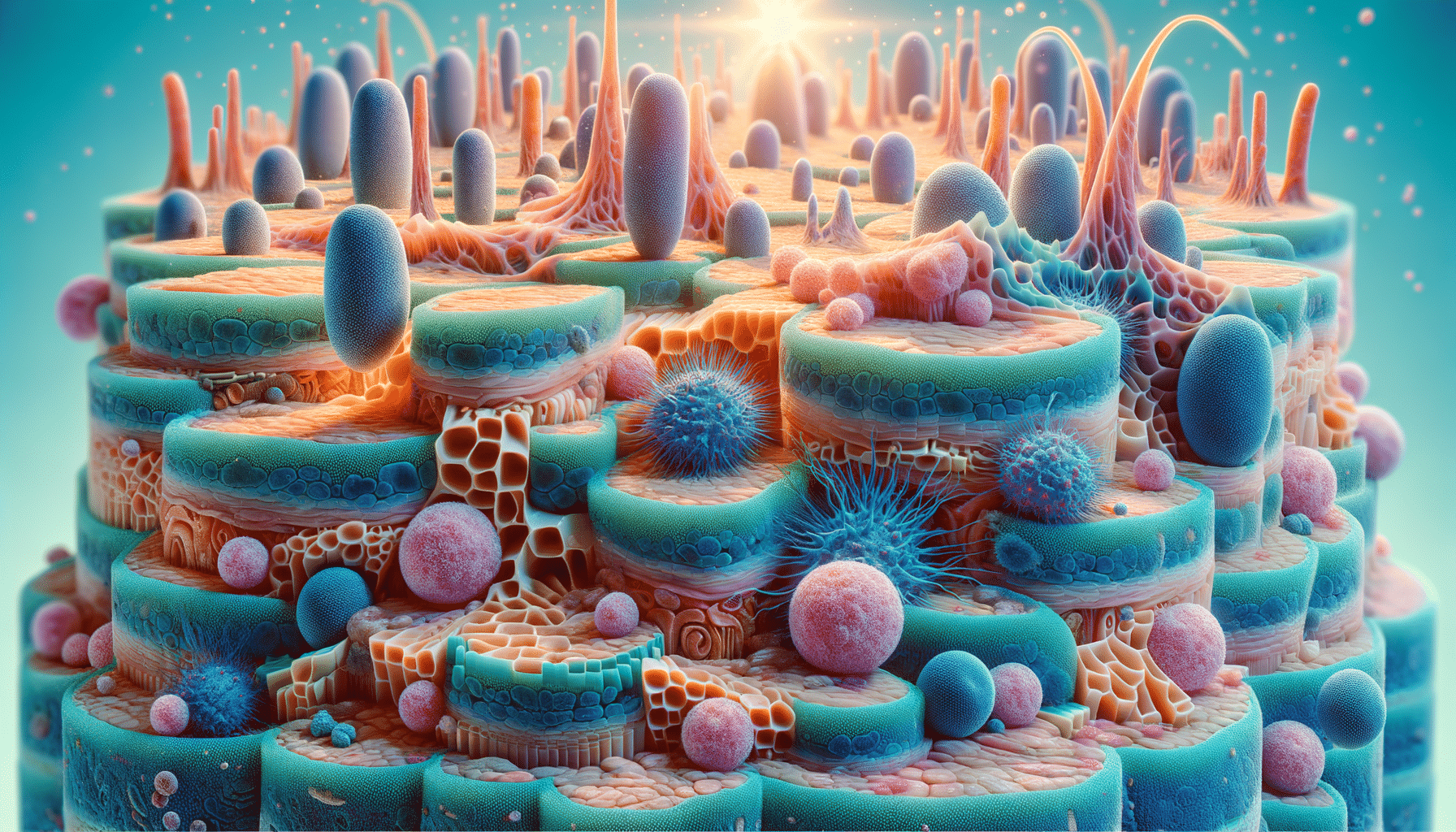
Autoimmune skin conditions are a group of disorders where the body’s immune system mistakenly attacks its own skin cells. These conditions can lead to a variety of symptoms, including rashes, blisters, and discoloration, significantly impacting an individual’s quality of life. Understanding these conditions is crucial for effective management and treatment, as they are often chronic and require long-term care.
The relevance of autoimmune skin conditions lies in their prevalence and the potential for severe physical and emotional effects. Conditions like psoriasis, lupus, and vitiligo are among the more well-known autoimmune skin disorders, each with unique characteristics and challenges. By delving into the specifics of these conditions, individuals can better recognize symptoms and seek appropriate medical advice.
Common Types of Autoimmune Skin Conditions
Autoimmune skin conditions encompass a range of disorders, each with distinct features. Some of the most recognized include:
- Psoriasis: Characterized by red, scaly patches on the skin, psoriasis is caused by an accelerated skin cell production process. It can affect various parts of the body and is often associated with joint pain, known as psoriatic arthritis.
- Lupus: A systemic autoimmune disease that can affect the skin, lupus often presents with a butterfly-shaped rash across the cheeks and nose. It can also cause lesions and increased sensitivity to sunlight.
- Vitiligo: This condition leads to the loss of skin pigment, resulting in white patches on different body parts. It occurs when the immune system targets melanocytes, the cells responsible for skin color.
Each of these conditions has a unique pathophysiology, but they share the commonality of being driven by the immune system’s erroneous attack on the body. The exact cause of these immune responses is not entirely understood, but genetic, environmental, and hormonal factors are believed to play significant roles.
Diagnosis and Management of Autoimmune Skin Conditions
Diagnosing autoimmune skin conditions often involves a combination of physical examinations, medical history reviews, and specialized tests such as blood tests and skin biopsies. Early and accurate diagnosis is essential for effective management, as these conditions can be persistent and progressive.
Management strategies typically focus on alleviating symptoms and preventing flare-ups. Treatment options may include:
- Topical Treatments: Creams and ointments, often containing corticosteroids, are commonly used to reduce inflammation and relieve symptoms.
- Systemic Medications: For more severe cases, oral or injectable medications that suppress the immune system may be prescribed.
- Phototherapy: Exposure to ultraviolet light can help slow skin cell growth and reduce symptoms for certain conditions like psoriasis.
In addition to medical treatments, lifestyle modifications can play a crucial role in managing autoimmune skin conditions. Stress management, a balanced diet, and avoiding known triggers such as certain foods or environmental factors can help maintain skin health and overall well-being.